keywords: Headache, Coronavirus Disease 2019, Personal Protective Equipment, Health Care Workers, N95 mask
Purpose: In the pandemic coronavirus disease 2019 (COVID-19), health care workers (HCWs) are at very high risk. Personal protective equipment (PPE) and masks are not only difficult to wear while working but also causes various complications. The present self-administered questionnaire- based study aimed to explore the headache and complications in HCWs on wearing PPE during the COVID-19 pandemic.
Methods: The present study was performed by obtaining a self-administered questionnaire from HCWs, which provides evidence of various complications due to the use of a PPE and mask.
Results: Out of a total of 329 respondents, 189(57.45%), 67(20.36%), 238(72.34%), 213(64.74%), 177(53.80%), and 34(10.33%) reported headache, breathlessness, suffocation, nose pain, ear pain, and leg pain respectively. Out of 329 respondents, 47(14.29%) had pre-existing headaches. Headache was significantly high for those who wore PPE for 4-6h (121/133; 87.05%) than that of those who wore up to 4h (18/26; 69.23%). Of the 34(24.46%) required medication who reported headaches wearing PPE. Acetaminophen is quite helpful in most health care workers to decrease headaches. Nose-related complications occur frequently in health care workers after regular shifts for more than 6 days. Gelatinous adhesives patch was a wonderful prophylactic remedy as it was helpful to prevent nose- related complications in 24 HCWs out of 25(96%).
Conclusions: More than half of the HCWs reported headache, suffocation, nose pain, and ear pain. Duration of PPE use of more than 4h is significantly associated with headache. Short duration PPE use prevent HCWs from headache and various ill effects.
Keywords: Headache, Coronavirus Disease 2019, Personal Protective Equipment, Health Care Workers, N95 mask
INTRODUCTION
In the pandemic coronavirus disease 2019 (COVID-19), health care workers (HCWs) are at very high risk. To prevent from COVID-19 infection health workers are using various kinds of personal protective equipment (PPE) kits and high-performance filtering masks(1).
PPE like N95/FFP2 or FFP3, surgical masks, face shields, and goggles are in various combinations with a PPE kit. It is not only causing discomfort but also cumbersome to wear a PPE kit, especially in ICU and high-risk zones like dialysis and emergency care(2).
There are still no clear guidelines about PPE use although WHO recommends usual 4-hour duration is optimal due to pandemics and less experience with the PPE, duration, and type of PPE use in different settings are not very familiar for HCWs(3). As they are working constantly without proper rest, diet, change in shifts, sleep deprivation, hygiene, and improper ventilation due to prolong use of filtering masks4) with PPE kit which may cause lead to fatigue, headache, nose pain, pain behind ears and on face and neck due to strings of masks and straps(5) of goggles causing compression(6). Skin problems include contact dermatitis due to frequent sanitizing and hand washing, moisture entrapped in gloves and due to profuse sweating with friction causing epidermal erosion. Leg pain, blurring of vision due to fog during the use of protective wear, dehydration due to sweating, and decreased intake during the time to this protective equipment increase fatiguability while work and after work.
Thus, we study the various difficulties faced by an HCW indifferent areas like ICU, emergency, sample collection areas, isolation ward, OPD, screening general ward, pharmacy, laboratory, and data collection areas of hospitals and also inquired about various experiences to cope up with these problems, as this pandemic will be going long and we have to work with these requirements with precautions so that we can work efficiently and dedicatedly to save the life of patients with minimum harm to HCWs.
METHODS
The present study was performed by obtaining a self-administered questionnaire from HCWs of different hospitals and medical institutes during the COVID-19 pandemic from 15 April 2020 to 15 October 2020. This questionnaire-based epidemiological study was approved by the Institutional Ethics Committee, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, India.
PPE including N95 mask, gown, and goggle with or without face shield was mandatory to wear in the COVID-19 ward, ICU, holding area, laboratory, and sample collection center, while N95 with or without face shield and goggle was used for protection in a general ward, dialysis laboratory and screening area.
Questionnaire
The questionnaire comprised demographics, past medical history, PPE usage patterns, pre-existing headache or de novo PPE-associated headache patterns, other difficulties due to PPE use, and PPE- associated personal experiences.
We obtained 381 responses out of 496 randomly distributed questionnaires from HCWs working in high- risk areas on COVID-19 duties, giving an overall response rate of 76.81%.
Based on participants' responses, we determined the use of PPE, goggle, face shield, type of face mask, a primary location where the PPE kit was worn, the average number of hours of each equipment used per day, the frequency of headaches, subtype (based on International Headache Society recommendations(7)), pre-existing headache, the severity of headaches, PPE associated suffocation, nausea, vomiting, nose pain, abrasion over the nose and ear pain, fogging, skin complications and medications used for relief.
Statistical Analysis
Data were expressed in mean±SD, median, or percentage. Data were analyzed using SPSS statistical software 17.0 (SPSS, Chicago, IL, USA). The percentage values in different groups were compared using Z-test as per the required application. P values ≤0.05 were considered significant.
RESULTS
Demographic Characteristics
Participants who have not signed the consent form (n=13) and replying incomplete responses (n=39) were excluded. Finally, 329 (265 males, mean age 35.83±9.24 years) of a total of 381 received responses were included in the final analysis of the study.
Out of 329 participants, 133 were doctors, 61 nurses, 60 technicians (laboratory, radiology, transfusion, dialysis), 8 researchers, and 67 attendants. Of the 329 HCWs, 159 (48%) wore PPE, and 132 (40%) uses the N95 face mask however 38(12%) wore a surgical mask. (Figure 1)
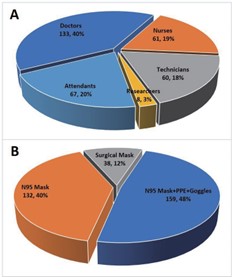
Figure 1. Demographic profile of Health Care Workers participating in the study during COVID-19 pandemic. Pei-diagram shows the Distribution of different HCWs provided self-administered questionnaire (A). Types of PPE used by Health Care Workers (B)
Out of 159, the duration of wearing PPE was 0-1h, 1-4h, and 4-6h in 9 (5.66%), 17 (10.69%), and 133(83.65%) respondents respectively. However, wearing duration of N95 mask only was 0-1h, 1-4h, 4-6h and 6-8h in 6 (4.55%), 19 (14.39%), 104 (78.79%) and 3 (2.27%) respondents. (Figure 2)
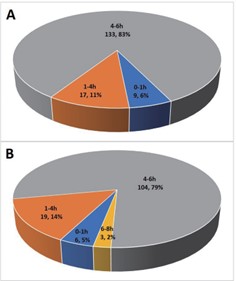
Figure 2. Duration of wearing PPE kit and mask by Health Care Workers participating in the study during COVID-19 pandemic. Pei-diagram shows the Duration of wearing N95 face PPE (A) and N95 mask only (B).
Headache
Of the 329 respondents, 189 (57.45%) reported headaches when they wore PPE. Of the 189 who reported headaches, 139 (87.42%) from 159 wore PPE; 46 (34.85%) from 132 wore an N95 face mask, and 4(10.52%) from 38 wore a surgical mask. (Table1)
Table 1. Complications associated with PPE kits and masks were noticed by Health Care Workers participating in the study during the COVID-19 pandemic.
|
Complications
|
N95 Mask+ PPE+ Goggles
|
N95 Mask
|
Surgical Mask
|
|
|
(N=159)
|
(N=132)
|
(N=38)
|
|
Headache
|
139(87.42%)
|
46(34.85%)
|
4(10.52%)
|
|
Breathlessness
|
43(27.04%)
|
24(15.09%)
|
-
|
|
Suffocation
|
145(91.19%)
|
93(70.45%)
|
-
|
|
Nose Pain
|
145(91.19%)
|
68(51.51%)
|
-
|
|
Ear pain
|
122(76.73%)
|
54(40.90%)
|
1(2.63%)
|
|
Itching
|
34(21.38%)
|
12(9.09%)
|
3(7.89%)
|
|
Fogging
|
154(96.86%)
|
78(59.09%)
|
-
|
|
Leg Pain
|
34(21.38 %)
|
-
|
-
|
|
Fatigue
|
124(77.99%)
|
9(6.82%)
|
-
|
|
Nausea
|
23(14.46%)
|
12(9.09%)
|
-
|
|
Weird Sensation
|
137(86.16%)
|
38(28.79%)
|
-
|
Out of 329 respondents, 47(14.29%) had a pre- existing headache (39 having migraine, 8 having TTH) and no one reported that a previous headache was associated with PPE and face mask in past. But during this Covid19 pandemic, 27 developed headaches due to frequent and prolonged PPE use. Seven respondents of them used to take medicine (three used flunarizine, two paracetamol, and two amitriptyline) for headaches, and the headache of others was cured on proper rest or sleep.
Headache in PPE wearing HCWs
Headache was started after donning PPE within 1h, 1-2h, 2-4h, 4-6h and after removal in 9 (7%), 25 (18%), 49 (35%), 43 (31%) and 13 (9%) respondents out of 139. Out of 139 who complained of headaches, 79(56.83%), 49(35.25%), and 11(7.91%) had mild, moderate, and severe headaches respectively. Of the 139 who complained of headaches on wearing PPE, the type of headache was continuous dull itching in 82 (58.99%), throbbing or pulsatile 25(17.98%), and band-like squeezing in 32(23.02%) respondents respectively. (Figure 3)
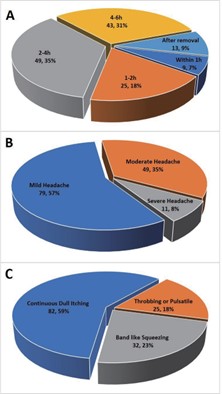
Figure 3. Duration, Severity, and Type of headache on wearing PPE kit and N95 face mask reported by Health Care Workers participating in the study during the COVID-19 pandemic. Pei- diagram shows Duration of headache started after donning PPE (A); Severity of headache (B) and Type of headache noticed by HCWs (C)
Location of headache
The location of headache was unilateral in 25(17.98%) and bilateral in 114(82.01%) who wore PPE. Of the 50(35.97%), 28(20.14%) and 5(3.59%) have only headaches in the frontal, lateral and occipital regions respectively; 29(20.86%) have only holocranial and 3(2.15%) have only on top of the head headache. However, 9(6.47%) have frontal and lateral region headaches; 6(4.31%) have lateral and occipital region headaches; 5(3.59%) have frontal and top of the head region headache and 4(2.87%) have lateral and top of the head region headache. (Figure 4)

Figure 4. Location of headache on wearing N95 PPE kit and N95 face mask reported by Health Care Workers participating in the study during COVID-19 pandemic. Pei-diagram shows Distribution of Unilateral and bilateral headaches in Health Care Workers on donning PPE kit and N95 face mask (A); Chart diagram represents the different locations of headache experienced by HCWs during COVID-19 duties(B).
There were 9 (6/50 of frontal and 3/9 of the frontal and lateral region) respondents who reported headaches due to tight straps of a mask, face shield, and goggles out of 139.
Duration of headache
Out of 139, the headache subsided within an hour and in 1-2h after doffing of PPE kit in 29(20.86%) and 80(57.55%) respectively. However, the headache persisted for one day, 5-7 days, and up to 2-3 weeks in 17(12.23%), 10(7.19%), and 3(2.15%) respectively after doffing of PPE kit. (Figure 5)
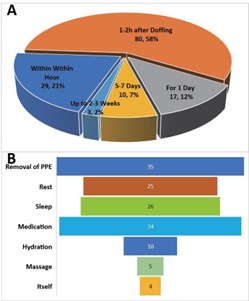
Figure 5. Duration of relief from headaches and Different ways by which to get relief from headaches were reported by Health Care Workers participating in the study during the COVID-19 pandemic. Pei- diagram shows Duration of relief from headache (A); Chart diagram represents Different ways by which get relief from headache reported by Health Care Workers during COVID-19 duties(B).
Type of headache
External-pressure headache 158(83.59%), Migraine with aura 2 (1.26%), Migraine without aura 22(11.6%), and Infrequent episodic TTH 3(1.58%).
Relief from Headache
Out of 139 who reported headaches 35(25.17%), 25(17.98%), 26(18.70%), 34(24.46%), 10(7.19%), 5(3.59%), and 4(2.87%) got relief from their headache by removal of PPE, rest, sleep, medication, hydration, massage and itself respectively. (Figure 5)
The number of respondents having a headache was significantly high those who wore PPE for 4-6h (121/133; 87.05%) than that of those who wore it up to 4h (18/26; 69.23%, p=0.002). Also, 5 respondents had to take leave for 2 days (1-4 days) for whose headaches persisted for a week.
Complications Associated with PPE and Mask
Out of the total of 329 respondents apart from headache, 67(20.36%), 238(72.34%), 213(64.74%), 177(53.80%), 49(14.89%), 232(70.52%), 34(10.33%) 133(40.43%) and 35(10.64%) reported breathlessness, suffocation, nose pain, ear pain, Itching, fogging, leg pain, fatigue, and nausea respectively. (Table1)
On assessing nose pain on the VAS scale, there were 32.41% and 55.88% of respondents had nose pain VAS (1-3) who wore PPE and N95 masks respectively and the difference was significant (p=0.001). There were 46.89% and 35.29% respondents who wore PPE and N95 masks only respectively with nose pain VAS (4-6), the difference was non-significant (p=0.111). However, having nose pain VAS (7-10), there were 20.68% and 8.82% respondents who wore N95 Mask+ PPE kit+ goggles and N95 mask respectively and the difference was significant (p=0.031). (Table 2)
Table 2. Nose pain on VAS scale in HCWs wearing PPE kit and masks in Health Care Workers during COVID-19 pandemic. The percentage of the Nose pain VAS scale (7-10) was significantly high those who wore N95 mask+ PPE kit+ goggle than that of those who wore N95 face mask only.
|
N95 Mask+ PPE kit+ Goggles
|
N95 Mask
|
|
Vas Scale
|
(N=145)
|
(N=68)
|
p-value
|
|
1-3
|
47(32.41%)
|
38(55.88%)
|
0.001
|
|
4-6
|
68(46.89%)
|
24(35.29%)
|
0.111
|
|
7-10
|
30(20.68%)
|
6(8.82%)
|
0.031
|
Contact dermatitis was also reported by 16(10.06%) HCWs who wore PPE. Two HCWs reported a small abscess behind the ear pinna. (Image 1)

Image 1. Representative pictures of Contact dermatitis and abscess behind pinna in Health Care Workers participating in the study during the COVID-19 pandemic. Representative pictures of HCWs showing Contact dermatitis on arm and fingers (A,B) and abscess behind pinna(C).
Eighteen (11.32%) out of 159 respondents who wore PPE reported injury on the nose surface due to heavy goggles and spectacles.
Precautionary measures before and while donning were taken by HCWs due to long shifts of 4-6 hours in PPE. Gauze piece was used over pinna or nose in about 50% of the respondents. Interestingly, 25 out of 27 HCWs who used gelatin-based adhesives reported help to prevent nose- related complications. Also 28(17.61%; 8 males, 20 females) HCWs used diapers for fear of urine.
DISCUSSION
We observed that most health care workers faced multiple problems with the use of PPE. Having an idea of these complications helps to use prophylactic measures to work smoothly in the high-risk zone and avoid these ill effects with these PPE.
Most respondents have the headache of external compression headache type as the time of onset and resolution after wearing or removing PPE is less than 60 minutes according to the definition of external compression headache.
The recommendation from WHO to use these masks is 4 hours(3). Suffocation and headache are most common. The prolonged duration tight fitting masks threads causing external compression which leads to more fatiguability and headache(5,6). Common location of headache was frontal, bilateral, holocranial, and posterior. Multiple different sites are also told by them like above pinna, temple, and behind the pinna. While blurring of vision due to fogging was found almost every health care worker used PPE along with N95 with goggles. The heavyweight of goggles adds more discomfort while working and it is the most aggravating factor for headache and fatiguability. Prolonged use of N95 or FFP2/FFP3 and goggles above the pin of the mask causes abrasion, pain, and swelling in different areas of the nose. Few notice abrasions on above and below pinna due to threads of straps of a mask. Prolonged use and multiple attempts to correct the position of masks and goggles to improve vision due to fogging, sweat, and secretion cause these abrasions. There is no way to remove sweat while a period of work causes irritability and decreases the efficiency of work. People also notice contact dermatitis while the use of PPE's most common reason was sweating and prolonged duration. Among the health care workers, prolonged use of protective equipment causes leg pain mostly after the first and second day of work schedule which improved itself after increasing fluid intake and proper rest after work. PPE should be used to decrease the risk of a mode of transmission as well as causing minimal discomfort to the HCW.
We found headache is less when PPE is used for less than 4 hours compared to more than 4 hours of use, which is found in other studies also(8,9). The cause of more headache in using PPE for more than 4 hours was reported due to hypoxiemia(10). As WHO recommends usual 4-hours duration is optimal(2). About 57% have a headache but only a minority required medication. The onset of headache within an hour after donning the PPE kit but that was mild pain while after 4 hours severity increased. Most of them experienced a dull type of headache even after removal. Few used analgesic medications occasionally while some experienced severe migraine-like headaches and must use analgesics for about a week regularly. Acetaminophen is quite helpful in most HCWs to decrease headaches. We observed headaches in a few cases due to tight straps and goggles causing supraorbital pain which are already reported the possible mechanisms(11) are inadequate ventilation(4) and External compression(12, 13) are also possible causes of headache.
One significant finding in our study was that abrasion and edema over the nose due to pressure from a pin of masks and load of goggles, occur frequently in HCWs when they do regular shifts for more than 6 days. Prophylactic use of gauze piece near pinna and near nose bridge was quite helpful to avoid nose-related complications and people experienced less fatigue after doffing, while gelatinous adhesives patch was wonderful prophylactic remedy as it was helpful to prevent nose- related complications in 24 HCWs out of 25(96%). As expected about 80% have intense thirst after 3 hours of PPE kit and about 28 HCWs used diapers for fear of urine while duty and 26% have the same fear. The urine control became more problematic after 4 hours as experienced by 34% of HCW irrespective of gender.
Few studies were done exclusively in ICU settings and they have not included health care providers who had avoided or been excused from working in such areas because of headaches, while in our study we included HCWs apart from ICU also. As there is a more stressful condition in ICU settings which may aggravate headaches and pain(14).
The only limitation of the study was the small sample size and recall bias however we did a questionnaire immediately after the duty to minimize this recall bias.
CONCLUSIONS
PPE and N95 masks will be required to manage COVID19, and their use may cause de novo external pressure headaches and exacerbation of migraine pain in patients. Four hours duration of wearing PPE may helpful for preventing HCWs by reducing headaches and other complications.
List of Abbreviation
COVID-19: corona virus disease 2019
HCWs: health care workers
PPE: personal protective equipment
ICU: intensive care unit
Acknowledgments: We are thankful to all Health Care Workers who participated in the study and share their honest experiences.
Disclaimers: None.
Disclosures: Nothing to disclose.
Conflict of Interest: There is no conflict of interest.
REFERENCES
- Hick JL, Thorne CD. Personal Protective Equipment. Disaster Medicine. 2006:246–54.
- Wong JEL, Leo YS, Tan COVID-19 in Singapore-Current Experience: Critical Global Issues That Require Attention and Action. JAMA. 2020 Apr 7;323(13):1243-1244.
- World Health Organisation. Rational use of personal protective equipment (PPE) for coronavirus disease (COVID-19). March2020. https://apps.who. int/iris/bitstream/handle/10665/331498/WHO-2019- nCoV-IPCPPE_use-2020.2-eng.pdf?sequence= 1&isAllowed=y.
- Cheshire, P., Jr and Ott, M.C. Headache in Divers. Headache: The Journal of Head and Face Pain, 2001;41: 235-247.
- Shenal BV, Radonovich LJ Jr, Cheng J, Hodgson M, Bender BS. Discomfort and exertion associated with prolonged wear of respiratory protection in a health care setting. J Occup Environ Hyg. 2012;9(1):59-64.
- Krymchantowski A, Barbosa JS, Cvaigman M, Lorenzatto W, Silva Helmet-related, external compression headache among police officers in Rio de Janeiro. Med Gen Med. 2004;6(2):45.
- Headache Classification Committee of the International Headache Society ( IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2018, 38(1)1–211.
- Lim EC, Seet RC, Lee KH, Wilder-Smith EP, Chuah BY, Ong BK. Headaches and the N95 facemask amongst healthcare providers. Acta Neurol 2006;113(3):199-202.
- Ong JJY, Bharatendu C, Goh Y, Tang JZY, Sooi KWX, Tan YL, Tan BYQ, Teoh HL, Ong ST, Allen DM, Sharma Headaches Associated with Personal Protective Equipment - A Cross-Sectional Study Among Frontline Healthcare Workers During COVID-19. Headache. 2020; 60(5):864-877.
- Kao TW, Huang KC, Huang YL, Tsai TJ, Hsieh BS, Wu The physiological impact of wearing an N95 mask during hemodialysis as a precaution against SARS in patients with end- stage renal disease. J Formos Med Assoc 2004; 103:624–8.
- Jacobson More "goggle headache": supraorbital neuralgia. N Engl J Med. 1983 Jun 2;308(22):1363.
- Headache Classification Subcommittee of the International Headache The International Classification of Headache Disorders, 2nd edn. Cephalalgia 2004;24(Suppl. 1):1–160.
- Fishbain Cervicogenic headache. Cephalalgia. 2002; 22(10):829; discussion 829-30.
14. Nash JM. Psychologic and behavioral management of tension-type headache: treatment procedures. Curr Pain Headache Rep
2003;7:475–81.