Purpose: The causes of acute stroke in patients with SLE are multifactorial. Antiphospholipid-associated hypercoagulability and inflammation-induced platelet activation are major causes of ischemic stroke in SLE patients. As such patients underwent intravenous thrombolysis and endovascular thrombectomy, they may have higher risk of complications and less favorable outcome.
Case Report: A 30-year-old woman with underline SLE and Takayasu arteritis who presented with right CCA and MCA occlusion status post rtPA and endovascular thrombectomy. Twelve hours after the procedure, head CT was ordered due to anisocoria with loss of pupillary light reflex. The head CT showed partial obliteration of suprasellar and quadrigeminal cistern due to extensive brain edema, leading to her decompressive craniectomy. Two days later, patient’s both pupil became dilated with head CT showing occlusion of the left MCA. Her condition drastically went downhill when complications such as central DI and myocardial stunning occurred.
Conclusion: Although autoimmune vasculitis is not listed as an absolute contraindication to endovascular thrombectomy, given the antecedent reports, it is prudent to disclose possible complications to both the patient and family while making the decision.
Keywords: SLE, arteritis, large vessel occlusion
INTRODUCTION
Large vessel vasculitides are systemic autoimmune diseases characterized by an initial inflammation of the large vessels, such as the aorta, and subsequent damage of the organ supplied by it. Prototypes of these vasculitides include temporal arteritis, Takayasu arteritis, and systemic lupus erythematosus (SLE). As an example, CNS manifestations of SLE patients include headache, cognitive dysfunction, mood disorders, psychosis, seizure, and cerebrovascular diseases(1). The causes of acute stroke in patients with SLE are multifactorial. Antiphospholipid- associated hypercoagulability(2,3) and inflammation- induced platelet activation(4) are major causes of ischemic stroke in SLE patients. Similar to the non-SLE population, hypertension was associated with intracranial hemorrhage, and the occurrence of cerebral aneurysm due to vascular fragility is associated with subarachnoid hemorrhage(4).
Literature has suggested that patients with SLE are prone to a 1.5- to 3-fold higher risk of ischemic stroke(5-7), 3-fold higher of intracranial hemorrhage, and 4-fold higher of subarachnoid hemorrhage(8) than the general population. Acute ischemic stroke has been estimated to cause 10-15% of mortality in patients with SLE(9).
This is a case report of a patient with SLE and Takayasu arteritis who presented with large vessel occlusive stroke and underwent intravenous thrombolysis and endovascular thrombectomy. However, her condition took a sharp turn when subsequent subarachnoid hemorrhage occurred and recurrent ischemic stroke on the contralateral side (of index event). The point to make is, although abided by all the guidelines, patients with SLE or other autoimmune vasculitides may have a higher risk of complications and poor outcomes when CNS is involved.
CASE REPORT
A 30-year-old Taiwanese woman with acute onset of left limbs weakness accompanied by slurred speech since 3 hours ago was brought into the emergency department by her family. Her significant past medical history includes SLE diagnosed since the age of 16 and has since been on prednisolone and tacrolimus, Takayasu arteritis diagnosed via vessel biopsy and severe right common carotid artery stenosis status-post drug-eluting stent placement at the age of 17, left eye blindness as a complication of the arteritis, and abdominal aortic aneurysm. She had pre-termed pregnancy at 35 weeks gestational age via cesarean section two years ago.
The patient presented to the emergency department within 4.5 hours of symptom onset, her consciousness was alert but mildly confused and able to obey commands and her initial NIHSS was 8 (bilateral left limbs weakness, facial palsy, and dysarthria). Neurologic exam revealed pupils equal (2.5/2.5mm) and reactive to light, rightward deviated gaze without extraocular movement limitations, left central facial palsy, dysarthria, tongue deviation toward left and left hemiparesis (MRC: 4). Her deep tendon reflexes were normal and bilaterally negative Babinski's sign.
Head CT with perfusion showed in-stent occlusion of the right common carotid artery and right middle cerebral artery (Figure 1). Perfusion scan revealed decreased CBV, CBF, and increased Tmax at the right MCA territory. Suspicious ischemic core about 88ml and hypoperfusion area about 197ml on the RAPID system. Per indication, the patient and families agreed to intravenous thrombolysis and subsequent endovascular thrombectomy (TICI 0-2a). Immediate postoperative head CT showed contrast extravasation and subarachnoid hemorrhage in the right Sylvian fissure, suprasellar cistern, and right cerebral cortex (Figure 2), thus prompting immediate ten units of cryoprecipitate. The neurosurgeon was consulted, and the patient was transferred to the neuro-critical care unit.
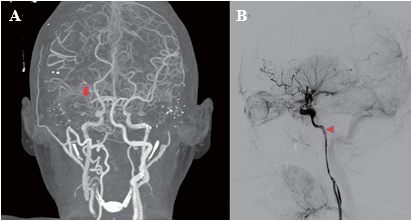
Figure 1. A) Head CT angiography with contrast showed occlusion of the right middle cerebral artery at M1 (arrow) with neovascularization serving collateral blood supply. B) carotid arteriography during endovascular thrombectomy showed lumenal stenosis (arrowhead) of the cervical and petrous part of the right internal carotid artery.
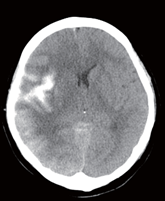
Figure 2. Follow-up head CT after endovascular thrombectomy found contrast extravasation and subarachnoid hemorrhage in the right Sylvian fissure, suprasellar cistern, and right cerebral cortex.
In the neuro-critical care unit, nicardipine pump was used to attain a strict systolic blood pressure goal of under 120 mmHg and a combination of mannitol and fentanyl to prevent worsening cerebral edema. Twelve hours after the endovascular thrombectomy, emergency head CT because of the presence of anisocoria (6.5/4.5mm) without light reflex. The CT scan showed a large area of hypodensity over the right cerebral hemisphere, generalized brain edema causing partial obliteration of suprasellar and quadrigeminal cisterns suggesting brain herniation, decompressive craniectomy ensued.
In consensus with the rheumatologist, considering that her ischemic stroke is likely related to SLE, Takayasu arteritis, and underlying autoimmune pathology. Thus, high-dose steroid and intravenous immunoglobulin (IVIG) therapy were given.
Two days after the craniectomy, her left pupil became dilated (6.5/6.5mm), which prompted another urgent head CT angiography. The result showed swelling of the right cerebrum and left frontotemporal lobes and iatrogenic carotid-cavernous sinus fistula (CCF) of the right side with a poor enhancement of right internal carotid artery, bilateral anterior and middle cerebral arteries (Figure 3). The situation was aggravated by myocardial stunning and central diabetes insipidus; subsequently, the patient crossed the point of no return despite aggressive medical treatment.
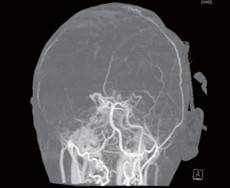
Figure 3. CT head angiography showed poor enhancement of the bilateral middle cerebral artery, suggesting the patient suffered from recurrent ischemic stroke with occlusion of the left middle cerebral artery.
DISCUSSION
Acute ischemic stroke due to autoimmune large vessel vasculitis remains a challenging topic. The patient passed away despite intensive medical and surgical treatment. Abiding by the current AHA/ASA guideline, the appropriate therapy for large vessel occlusive ischemic stroke is intravenous thrombolysis and endovascular thrombectomy in qualified patients. However, the outcome is unpredictable, ranging from near-complete recovery to permanently disabled or even mortality. Although the current guideline for acute ischemic stroke treatment is constructed on top of evidence found in world-renowned research, none scrutinized the outcome in patients with large vessel autoimmune vasculitis.
A recent report discussed the clinical conundrum in the management of acute ischemic stroke in Takayasu arteritis (TA). A multicenter case-controlled study of 17 TA patients with stroke showed that the middle cerebral artery is the most commonly affected intracranial artery (n=12), stroke was diagnosed in 4 patients who underwent internal carotid operation(10). A plethora of underline mechanisms may have contributed to stroke in TA; endothelial injury may lead to vascular occlusion or the formation of aneurysms, altered blood flow dynamic due to vessel stenosis or steal phenomena, secondary moyamoya syndrome, and renovascular hypertension10. The involvement of the carotid artery serves as the major cause of stroke in this population, and vascular intervention is often required in acute treatment. However, the rate of restenosis following stent placement is relatively high (37% to 62%)(11). Therefore, long-term use of immunosuppressants, anticoagulants, or antiplatelets is crucial in the secondary prevention of stroke. However, in reality, these pharmacological treatments are often given in the reduced dose due to vascular fragility and high bleeding risk, and there is yet a consensus among experts.
Patients with SLE-related large vessel occlusive stroke face multiple comorbidities, such as antiphospholipid syndrome, vasculitis, and Libman Sacks endocarditis. They are compounded by the activation of proinflammatory cytokines(12-14), leading to endothelial dysfunction and a higher risk of hemorrhage8. While there are no large-scale studies, several case reports have observed complications such as hemorrhagic transformation(15), intracranial hemorrhage(16), or recurrent ischemic stroke during index hospitalization(15).
Immunosuppressive therapy is often used to control the inflammatory activities in patients with autoimmune vasculitis; however, its use could also contribute to an increased risk of ischemic and hemorrhagic strokes. Corticosteroids and calcineurin inhibitors may all contribute to elevated serum cholesterol levels(17) and thus increased risk of vascular events. Although yet to be elucidated, in vitro experimental results showed that tacrolimus promotes collagen-induced platelet aggregation and inhibits thrombin-induced platelet aggregation(18). A recent case report of post-liver transplant patient on tacrolimus developed reversible posterior encephalopathy syndrome (PRES) and intracranial hemorrhage(19). One of the suggested pathomechanism may be related to tacrolimus-induced nitric oxide synthesis impairment(20), leading to vasoconstriction and blood-brain barrier dysfunction.
Lastly, patient developed CCF was most likely related to mechanical thrombectomy, although the occurrence of iatrogenic CCF is rare(21), but this patient may be at higher risk of iatrogenic CCF due to vessel fragility.
Stroke is a major cause of disability in patients with autoimmune vasculitis, the disease itself and the pharmacologic therapy both plays a significant role in the development of vascular events. Thus, there is a need for further studies to evaluate the prognosis of vasculitides related to large vessel occlusive stroke and identify possible predictors of functional outcome in the setting of endovascular thrombectomy.
CONCLUSION
Autoimmune vasculitis contributes significantly to acute stroke in the young population, increased risk of all types of stroke. Furthermore, multiple comorbidities and the chronic use of immunosuppressive medications dictates subsequent complications and outcome. Although autoimmune vasculitis are not listed as an absolute contraindication to endovascular thrombectomy, given the antecedent reports, it is prudent to disclose possible complications to both the patient and family while making the decision.
REFERENCES
- Ainiala, Hanna, et "The prevalence of neuropsychiatric syndromes in systemic lupus erythematosus." Neurology 57.3 (2001): 496-500.
- Hanly, G., et al. " Short-term outcome of neuropsychiatric events in systemic lupus erythematosus upon enrollment into an international inception cohort study." Arthritis Care & Research: Official Journal of the American College of Rheumatology 59.5 (2008): 721-729.
- Valdés-Ferrer, Sergio I., et al. "Cerebral Changes in SLE With or Without Antiphospholipid Syndrome. A Case-Control MRI Study." Journal of Neuroimaging 18.1 (2008): 62-65.
- Guraieb-Chahin, , et al. "Stroke in systemic lupus erythematosus: epidemiology, mechanism, and long- term outcome." Lupus 29.5 (2020): 437-445.
- Chiu, Chun-Chih, et al. "Increased risk of ischemic stroke in patients with systemic lupus erythematosus: a nationwide population-based " Internal Medicine 51.1 (2012): 17-21.
- Wang, I-Kuan, et "Risks, subtypes, and hospitalization costs of stroke among patients with systemic lupus erythematosus: a retrospective cohort study in Taiwan." The Journal of rheumatology 39.8 (2012): 1611-1618.
- Arkema, Elizabeth , et al. "Stroke in systemic lupus erythematosus: a Swedish population-based cohort study." Annals of the rheumatic diseases 76.9 (2017): 1544-1549.
- Holmqvist, Marie, et "Stroke in systemic lupus erythematosus: a meta-analysis of population-based cohort studies." RMD open 1.1 (2015): e000168.
- Cervera, Ricard, et "Morbidity and mortality in systemic lupus erythematosus during a 10-year period: a comparison of early and late manifestations in a cohort of 1,000 patients." Medicine 82.5 (2003): 299- 308.
- Couture, Priscille, et "Cerebrovascular events in Takayasu arteritis: a multicenter case-controlled study." Journal of Neurology 265.4 (2018): 757-763.
- Gao, Peng, et al. "Contemporary Challenges of Acute Ischemic Stroke in Takayasu Arteritis." Stroke 51.10 (2020): e280-e284.
- Bertsias, George , Jane E. Salmon, and Dimitrios Boumpas. "Therapeutic opportunities in systemic lupus erythematosus: state of the art and prospects for the new decade." Annals of the rheumatic diseases 69.9 (2010): 1603-1611.
- McMahon, Maureen, e t a l . "Dysfunctional proinflammatory high-density lipoproteins confer increased risk of atherosclerosis in women with systemic lupus " Arthritis & Rheumatism: Official Journal of the American College of Rheumatology 60.8 (2009): 2428-2437.
- O'Neill, Sean G., et al. "Antibodies to apolipoprotein A-I, high-density lipoprotein, and C-reactive protein are associated with disease activity in patients with systemic lupus " Arthritis & Rheumatism 62.3 (2010): 845-854.
- Shih, Yu-Cheng, et "A challenging case of neuropsychiatric systematic lupus erythematosus with recurrent antiphospholipid-related stroke: A case report and literature review." Neurology international 11.3 (2019): 40-43.
- Fattahi, Pooia, et al. "Thrombolysis for acute stroke in patients with vasculitis: case report and literature discussion." Clinical neurology and neurosurgery 115.3 (2013): 351.
- Agarwal, Arnav, and GV Ramesh Prasad. "Post- transplant dyslipidemia: mechanisms, diagnosis and " World journal of transplantation 6.1 (2016): 125.
- Wang, X., L. Zhao, and K. "In vitro effects of tacrolimus on platelet function." Zhonghua xue ye xue za zhi= Zhonghua Xueyexue Zazhi 35.10 (2014): 905- 908.
- Chen, Xiaoqian, Weixue Zhu, and Suhua Jiang. "A case report of reversible posterior encephalopathy syndrome with intracranial hemorrhage in a " Medicine 100.12 (2021): e25266.
- Cook, Leslie , et al. "Tacrolimus reduces nitric oxide synthase function by binding to FKBP rather than by its calcineurin effect." Kidney international 75.7 (2009): 719-726.
- Grüter, Basil , et al. "Carotid-cavernous sinus fistula following mechanical thrombectomy in acute ischaemic stroke: a rare complication." Neuroradiology (2021): 1-4.